Abstract
Introduction
Anticoagulants (AC) are commonly used for primary prevention of venous thromboembolism (VTE) in hospitalized patients. Mechanical methods of VTE prevention such as sequential compression devices (SCD) are used mostly in combination with AC or in patients with high risk of bleeding.
Objective
To determine if the use of SCD prevents VTE in medically ill hospitalized patients.
Methods
All Sparrow Main Hospital admissions from 04/01/2015 to 03/31/2016 were included and categorized according to the methods used for prevention of VTE- SCD only (SCD), anticoagulants only (AC), SCD & anticoagulants (BOTH), and none (NONE). We excluded patients less than 18 years of age and those with VTE on admission. Bivariate and multivariate regression analyses were conducted. To control for the selection bias of patients to SCD, AC or BOTH group, we performed propensity score matching. First, the propensity scores for SCD, AC, and BOTH were estimated using logistic regression. The 1-1 optimal matching method was used to find matched controls from patients without treatment. The matched samples are expected to mimic the randomized controlled trial.
Results
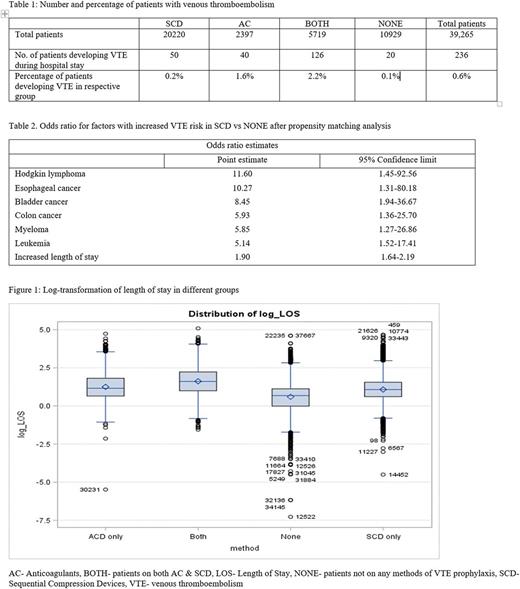
We identified a total of 39,265 eligible patients for our study- 20,220 of them were on SCD for VTE prophylaxis, 2,397 had AC, 5,719 had BOTH, and 10,929 had NONE of the measures (Table 1). Out of them, 0.6% (n=246) developed VTE during their hospital stay- 50 patients in SCD group, 40 in AC, 126 in BOTH, and 20 in NONE group. Among patients in the SCD group, 0.2% developed VTE; 0.1% developed VTE in NONE group. VTE developed in 1.6% of cases in the AC group and 2.2% in BOTH group (Table 1).
Among patients without VTE, mean age was 56 years (SD±20.3), 58% were females, and 55% were active/former smokers. Similarly, patients with VTE had mean age of 62.7 (SD± 16.4); 44.5% were females and 52.5% were smokers. Mean length of hospital stay was 4.3 days (SD±5.5) in patients without VTE compared to 11.5 days (SD±12.82).
Before propensity score matching, analysis showed that the risk of VTE was not decreased in SCD group compared to NONE group (OR 1.22, 95% CI 0.65-2.29). However, propensity matching analysis actually showed that the odds of developing VTE decreased with SCD compared to NONE (OR 0.26; 95% CI 0.18-0.38).
Multivariate analysis showed various cancer types were associated with higher odds of VTE while comparing SCD vs NONE (Table 2). Hodgkin lymphoma had the highest risk among them (OR 11.60; 95% CI 1.45-92.56), followed by esophageal cancer (OR 10.27; 95% CI 1.31-80.18), bladder cancer (OR 8.45; 95% CI 1.94-36.67), colon cancer (OR 5.93; 95% CI 1.36-25.70), myeloma (OR 5.85; 95% CI 1.27-26.86), and leukemia (OR 5.14; 95% CI 1.52-17.41). Increased length of stay also led to increased VTE (OR 1.90; 95% CI 1.64-2.19).
Conclusion
Use of SCD prevents VTE during hospital stay. However, other confounding factors may also play a significant role. More studies to define role of SCD in VTE prevention are needed. Regardless of the method used for prevention, increased length of stay is associated with increased risk of VTE.
Dhakal: Graduation Medical Education, Inc., Michigan State University: Research Funding. Rayamajhi: Michigan State University, College of Education: Research Funding; Sparrow/MSU Center for Innovation and Research: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.